
Diabetes mellitus is a common disease that perhaps every adult has heard of. It can be congenital or acquired during life, but in any case it is chronic and does not have a total cure. Many have heard that diabetes is not a disease but a way of life. After all, the patient must follow a special diet for life and use individually selected medications, not always insulin injections. In general, nutrition in diabetes mellitus cannot be considered a diet in the broad sense of the word, because there are not as many restrictions on it, and most prohibited products can be replaced with similar flavor properties, but safe for a person's sensitive body. diabetic.
What is diabetes mellitus and its types
Diabetes mellitus is a chronic disease in which there is a violation of glucose metabolism. It may be a consequence of a decrease in the amount of the hormone insulin produced by the cells of the pancreas, then type 1 diabetes mellitus (insulin dependent) is diagnosed, or it becomes the result of regular overeating leading to obesity, severe stress and others. factors, then type 2 diabetes mellitus (non-insulin dependent) develops.
Insulin is a biologically active substance released into the blood, capturing a glucose molecule and transporting it to the desired cells.
It is type 2 diabetes that is most diagnosed today and requires more attention from doctors, in addition to adherence to special dietary principles, as it becomes a consequence of the unhealthy lifestyle that the person leads. With the regular intake of a lot of carbohydrates in the body, the pancreas works to wear out and eventually either ceases to handle its function or produces "damaged" insulin that the cells and tissues don't notice. This means that this insulin is not able to capture the glucose and transport it to its destination, since the cells "don't see it", ie. develops insensitivity to it. The least role in this is played by changes in the hormonal background that inevitably come with age.
In both cases, there will be a marked increase in the concentration of glucose (sugar) in the blood and the development of characteristic symptoms:
- increased thirst;
- dry mouth;
- weakness;
- deterioration of vision;
- increased appetite, etc.
Type 2 diabetes mellitus is diagnosed more frequently, namely in 85-90% of patients. It usually occurs after 40 years and especially often after 65 years. This susceptibility of the elderly to the development of carbohydrate metabolism disorders is a consequence of the decrease in physical activity and the decrease in muscle mass, the main consumer of glucose, and abdominal obesity increasingly observed is becoming an additional factor that increases the risk of develop non-insulin dependent diabetes.
Abdominal obesity is the predominant deposition of adipose tissue in the abdomen.
Diagnosing diabetes is not difficult. For this, a blood glucose test is performed. Obtaining increased indicators serves as a reason for further examination and selection of optimal treatment tactics, one of the mandatory components of nutritional correction.
Why It's Important to Follow Basic Nutritional Principles
In any type of diabetes mellitus, the blood sugar level rises, but despite this, the cells cannot receive it due to insulin deficiency or the development of insulin resistance. As glucose is a monosaccharide that breaks down carbohydrates, it acts as the body's main source of energy. Therefore, if the tissues do not receive it in sufficient quantity, they starve, which, due to the transmission of the corresponding nerve impulses to the brain, leads to the appearance of a similar sensation in man. Therefore, with diabetes, patients may feel like eating something, especially sweet, even an hour after a healthy meal.
As a result, patients overtly eat high-calorie carbohydrate foods, which, in type 2 diabetes mellitus, quickly lead to weight gain and progression to obesity. This leads to an even greater jump in blood glucose levels, an increase in pancreas load, an increase in insulin production, an increase in tissue resistance to it, an aggravation of the condition, ie, the formation of a virus vicious circle.

In such situations, if you do not intervene in a timely manner and break this cycle, high sugar levels (hyperglycemia) will lead to the development of ketoacidosis and diabetic coma. Initially, the patient will feel strong thirst and will often go to the bathroom, then weakness, shortness of breath will quickly combine, a characteristic acetone smell from the mouth and urine will appear, nausea and vomiting will occur. In the absence of competent medical care, confusion and, ultimately, diabetic coma will occur.
In addition, long-term uncontrolled (uncompensated) diabetes mellitus can lead to the development of:
- retinal lesions with subsequent irreversible blindness;
- impaired kidney function and chronic kidney failure;
- poorly healed trophic ulcers on the legs, which are very difficult to treat;
- osteoporosis, with the possibility of fracturing any of the bones of the skeleton, including the spine, even with minimal impact;
- disorders of the heart and blood vessels, organs of the digestive tract, etc.
Therefore, it is important not only to diagnose diabetes mellitus in time and to take the medications prescribed by the endocrinologist, but also to strictly follow dietary recommendations.
Diet characteristics
The diet for type 1 and type 2 diabetes mellitus has some differences that patients should understand. With regard to nutrition for insulin-dependent diabetes, where patients receive lifelong replacement therapy in the form of regular insulin injections, doctors in different countries see the need to limit simple carbohydrates in different ways.
Foreign endocrinologists believe that it is not necessary to reduce the amount of their consumption in type 1 diabetes with properly selected insulin therapy. Home doctors believe that this has undesirable consequences and insist on the need to limit consumption of simple carbohydrates, but not abandon them completely, as in non-insulin-dependent diabetes. In type 2 diabetes mellitus, such disputes are inadequate, as the use of sugar can have dire consequences with it, which is not questioned in any country.
In addition, people with type 1 diabetes must be able to count bread units (XE), and people with type 2 diabetes must be able to determine the glycemic index (GI). Nutrition should be structured so that these daily diet indicators correspond to developed norms.
Therefore, today with diabetes mellitus, patients receive the so-called diet #9 in several modifications, the differences of which are insignificant. Which table is most suitable for a particular patient is determined by the endocrinologist, based on the test results and the person's condition.
In general, Diet #9 is designed to normalize carbohydrate metabolism, reducing the amount of simple carbohydrates consumed and, consequently, lowering the blood glucose level. With this, it is possible to normalize the amount of sugar in the blood, prevent the development of possible disturbances in the metabolism of fats and complications of the disease.
Diet #9 assumes a complete rejection of simple carbohydrates in the context of daily consumption of no more than 300 g of complex carbohydrates, while keeping the amount of protein foods within the physiological norm.
Basic nutritional principles
In case of diabetes mellitus of any type, the following recommendations must be observed:
- food must certainly be divided and consist of at least 5 meals, mainly in the insulin-dependent form;
- breakfast is a must-have meal;
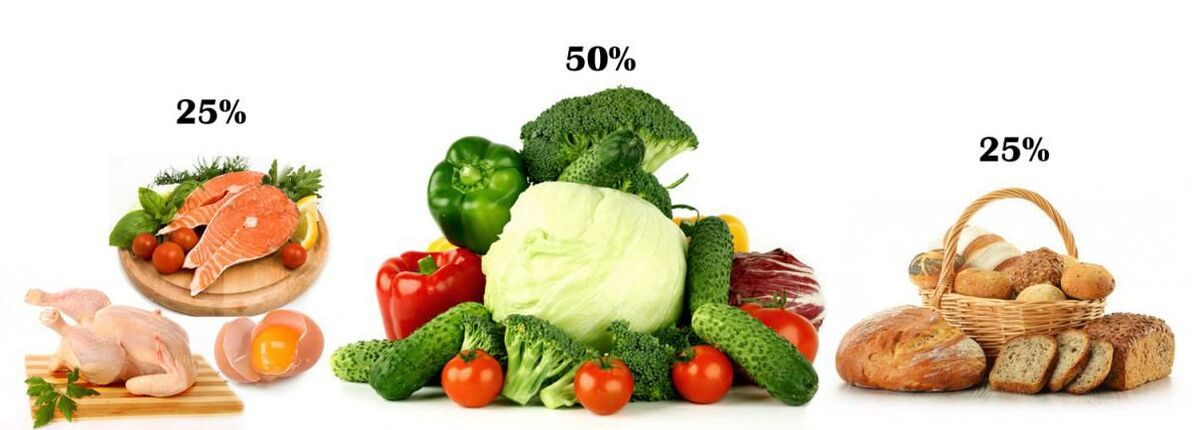
- in the preparation of the menu, the physiological proportion of proteins (meat, fish, dairy), carbohydrates (cereals, bread) and vegetables must be respected, which must represent 25%, 25% and 50%, respectively;
- The nutritional advantage is always given to foods with a low glycemic index and a high percentage of vegetable fiber;
- each meal starts with vegetables and protein is left at the end;
- the amount of salt should not exceed 5 g per day;
- fasting for diabetes is prohibited, if necessary, to reduce weight, this is done by increasing physical activity;
- when choosing a method of cooking vegetables, it is recommended to prefer minimal heat treatment or to abandon it completely, boiling, roasting and steaming are ideal;
- A vegetarian diet for diabetes is not the best choice, although it helps to improve the course of the disease and increase insulin sensitivity, you can only change it with the permission of an endocrinologist.
Nutrition for type 1 diabetes
Insulin-dependent diabetes is usually diagnosed in childhood. Since the cause of its development is the destruction of the cells in the pancreas that synthesize insulin, patients should be prescribed insulin therapy, and the drug and dosage selected individually. Insulin injections completely cover the deficit in hormone production in the body, so significant dietary restrictions are not necessary, but the child's parents, and then himself, must learn to correctly calculate the amount of carbohydrate consumed to match the dose. of administered insulin. To this end, tables were created specifically indicating the number of so-called grain units in each product.
In type 1 diabetes mellitus, it is only necessary to refuse:
- any sugary drinks, including juices;
- pre-cooked breakfast cereals;
- confectionery.
You cannot eat more than 7XE per meal and up to 25XE per day. In this case, the amount of all carbohydrates ingested per serving volume is added up. For example, 2 XE is contained in 3 tbsp. me. finished noodles, 4 tbsp. me. rice, 14 tbsp. me. vegetables or 420 g of tomatoes.
1 XE is equal to 12 g of carbohydrates or 20 g of bread.
Sweets are not strictly prohibited, but only those who control their blood glucose several times a day can buy them, accurately count XE and independently regulate the dose of insulin administered.
In severe type 1 diabetes mellitus, patients are given diet #9b and large doses of insulin. It involves the use of 400-450 g of carbohydrates and is very close to the diet of most modern people. It is allowed to consume 20-30 g of sugar per day.
The endocrinologist who monitors the patient's condition will certainly tell you how to distribute the amount of food between the individual doses, depending on the type of medication prescribed. Thus, with the introduction of insulin twice a day (in the morning and in the afternoon), it is necessary to compose the menu so that almost 2/3 of the total daily carbohydrate intake falls at this time. Also, after each injection, you need to eat 2 times - 15 minutes after the injection and 3 hours later. Fractional nutrition and controlling the amount of XE are the basis of the diet for type 1 diabetes.
If, after the injection, the patient suddenly feels weak, this indicates a deficiency of glucose in the body. In such situations, you should immediately eat a piece of dark chocolate.
Thus, in the insulin-dependent form of the disease, the main difficulty lies in the need to control not the type of food, but its volume and count the units of bread.
Nutrition for type 2 diabetes
In most cases, obesity is the main cause of the disease. Therefore, the type 2 diabetes diet is the first and main component of the treatment and prevention of complications. With their help, it will be possible to normalize sugar levels and control weight, thus preventing unwanted changes and worsening of the condition.
All patients need to independently monitor their blood glucose levels daily using home glucometers, and if stable high rates are achieved, consult a physician immediately.
If the patient is diagnosed with a mild or moderate insulin-independent form of the disease, and their weight is within the normal range, they receive staple diet #9 with a daily caloric intake of up to 2500 kcal. In these situations, you cannot consume more than 275-300g of complex carbohydrates from different sources per day.
In the presence of obesity, it is necessary not only to maintain the glucose level within the normal range, but also to reduce weight, since its excess negatively affects the effectiveness of the treatment and the patients' well-being. Therefore, in these cases, patients are prescribed the so-called reduced diet No. 9, which is characterized by a reduction in caloric content due to an even greater restriction on the permitted amount of complex carbohydrates consumed daily. In this case, the endocrinologist individually calculates this rate based on the degree of obesity. Therefore, in different cases, patients can consume from 100 to 225 g of carbohydrates, and the total caloric intake should not exceed 1700 kcal per day.
what is not allowed
Thus, in type 2 diabetes mellitus, it is necessary to completely exclude from the diet foods that contain the so-called fast carbohydrates, that is, those that are broken down into glucose and absorbed into the bloodstream within 15 minutes. They give you an energy boost quickly, but don't create a feeling of fullness, so after eating them, hunger quickly returns. These include:
- sugar;
- Honey;
- Confectionery, Classic Pastry;
- ice cream, chocolate;
- marmalade, jam, jam, jam;
- sweet vegetables, fruits, berries (grapes, bananas, dates, pineapples, persimmons, dried fruits);
- white bread, bread;
- semolina;
- smoked meats, fatty dishes;
- Mayo;
- fast food, snacks.
For diabetics, special recipes were created, including permitted products, for baking.
Diet number 9 does not require complete rejection, but recommends minimizing the amount consumed as much as possible:
- potatoes;
- beetroot;
- corn;
- carrots;
- soy products;
- pasta;
- of bread.
If you are obese, you will need to completely abandon all high-fat foods:
- butter and vegetable oil, spreads;
- sour cream, full-fat cheeses, cottage cheese, cream;
- lard, fatty meat and fish, chicken with skin;
- Nut seeds;
- alcohol, etc.
In these situations, it is recommended to replace these products with vegetables that have a beneficial effect on carbohydrate metabolism. They are green leaves, eggplants, cucumbers, turnips, cauliflower, pumpkin, zucchini, radishes, etc.
It is imperative to try to completely abandon foods with a high amount of fat, in particular canned foods, products from the meat processing industry, storage sauces. They are replaced by cooked or cooked dietary meats (chicken, rabbit, turkey, low-fat yogurt without additives).
what can
Carbohydrates are an indispensable part of the daily diet and should be on the diabetes menu, but only in acceptable amounts. Patients can only eat foods with slow absorbing carbohydrates and high fiber content. This:
- vegetable;
- wholemeal bread with bran;
- whole grains (8-10 tablespoons), with the exception of refined rice.
Since sugar in any form is prohibited for diabetics, its non-glucose substitutes were specially created. Many of them are many times sweeter than sugar and can be used in minimal amounts. Modern sweeteners include xylitol, stevia, sorbitol, fructose. But studies have shown that some of them can have a negative effect on the body. Stevia is considered the safest sugar substitute today. It is obtained from natural raw materials and in sweetness it surpasses sugar by 10-30 times (depending on the form of release: a powder of an herb or an extract called stevioside).

It is important that patients know the glycemic index of foods. Today, there are special tables that help to navigate the choice and correctly calculate the allowable consumption rate. In diabetes, preference should be given to foods with a GI lower than 55 (apples, cucumbers, cherries, broccoli, lettuce, milk, cauliflower, etc. ). They break down slowly and lead to little or no increase in blood sugar levels. These products can be consumed up to 200 g during a meal, but preferably together with protein foods.
Heat treatment increases the GI.
It is allowed to use:
- potatoes (not more than 200 g per day);
- meat and vegetable broth dishes;
- lean meats and fish (chicken, turkey, julienne, pike, hake);
- lentils;
- fermented low-fat milk and dairy products, cheeses with less than 30% fat content;
- eggs (3-4 per week, but no more than 1 per day);
- vegetable oil (no more than 1 tablespoon. L. per day);
- Special sweets, waffles, breads for diabetics.
When making homemade jams, sweeteners are added instead of sugar.
Nutrition for gestational diabetes
Pregnant women with a genetic predisposition to developing diabetes mellitus may face the development of so-called gestational diabetes within 20-24 weeks. It arises in the context of the presence of a reduction in hereditary tissue sensitivity to inulin, amplified by hormones produced during pregnancy in increased amounts: estrogen, prolactin, cortisol. They are able to block insulin and cause blood sugar to rise.
Often, after delivery, carbohydrate metabolism gradually returns to normal as the hormonal background normalizes. However, if the basic principles of feeding and feeding are not followed, there is not only the risk of preserving diabetes mellitus, but also the development of complications that can lead to premature birth, pyelonephritis in the mother, pathologies of the fundus of the eye. , as well as complications during childbirth. It is with the aim of early detection of gestational diabetes during pregnancy that regular blood glucose tests are performed and, if hyperglycemia is detected, a diet is prescribed.
In such situations, women are advised to:
- completely exclude simple carbohydrates from the diet (the same sugar, confectionery, chocolate, sweets, white and black bread, bananas, grapes, juices, dried fruits, etc. );
- limit your intake of complex carbohydrates to your doctor's recommended amounts;
- remove most of the daily diet from vegetables, unsweetened fruits;
- refuse to eat fatty foods, fried foods, semi-finished products, a variety of sausages, smoked products;
- when choosing a method of cooking the products, give preference to roasting, stewing, steaming;
- eat in fractions, preferably every 2 hours, highlighting 3 main meals (breakfast, lunch and dinner), as well as 2 additional ones (second breakfast, afternoon snack);
- drink at least 1. 5 liters of water.
Pregnant women with gestational diabetes are advised to measure their blood sugar after each meal.

All of these recommendations are relevant to the postpartum period. In either case, for the first few months of a baby's life, a breastfeeding woman is forced to follow a hypoallergenic diet and refuse fatty, fried foods. The same diet will help eliminate gestational diabetes and prevent its transition to a chronic carbohydrate metabolism disorder within 2-3 months of giving birth. If, after this period of time, the blood glucose level does not return to normal, the woman needs to consult an endocrinologist for examination and development of treatment tactics.
Sugar reducing products
There are several foods that can help lower blood glucose levels. They are called hypoglycemic and are recommended for patients with diabetes mellitus. But since each person is a unique biological system and has individual characteristics, he can react to certain types of food in his own way, and not just cause allergic reactions. Therefore, although glucose-lowering foods can provide invaluable help to patients with diabetes mellitus, especially type 2 diabetes, it is worth consulting an endocrinologist before starting their daily use.
Therefore, sugar reducing foods include:
- Cherries (GI 22) - contains anthocyanin, which helps to lower blood sugar and blood pressure, in addition to eliminating the so-called bad cholesterol. The daily norm is 100 g.
- Grapefruit (GI 29) - Contains naringin, a powerful antioxidant that helps increase tissue insulin sensitivity. It is recommended to consume 1 medium grapefruit or freshly squeezed juice per day (commercial not suitable). But grapefruit can adversely affect the quality of absorption of many medications, so you should consult your doctor before adding it to the menu.
- Cinnamon is a source of polyphenols that help keep blood sugar levels under control. The daily fee is 1/2 tsp. It can be added to cottage cheese, oatmeal and is very suitable for making casseroles with apples.
- Broccoli is a valuable source of fiber, so beneficial for diabetes, and the substances it contains help to slow down the rate of sugar absorption in the intestine. The daily norm is 200 g.
- Blueberries are one of the healthiest foods for diabetics, as they contain valuable glycosides, tannins and anthocyanins, which help maintain normal glucose levels and reduce the risk of developing diabetic retinal damage. The daily norm is 200 g.
- Oats and millet porridge are high in fiber, which helps maintain sugar levels.
- Jerusalem artichoke is a natural source of insulin, so its use contributes to the normalization of glucose levels, and the presence of fructose in the composition provides a pleasant sweet taste, which allows its use raw or added to salads.
- Garlic is one of the healthiest foods for everyone as it contains many antioxidants, natural antibacterials and other substances. Its use makes the pancreas work more actively, which is very valuable for patients with type 1 diabetes.
- Fish - Diabetic fish usually eat at least twice a week and, whenever possible, try to replace meat dishes with this food. It helps to normalize sugar levels and also to obtain essential polyunsaturated fatty acids.

Thus, the diet for diabetes mellitus can be varied and tasty. With a competent approach to menu planning, it won't cause rejection, but instead will help to increase energy and efficiency, as it largely corresponds to rational eating principles. But remember that it's important in diabetes to maintain a normal level of physical activity, as exercise increases tissue sensitivity to insulin.

































